Purulent-septic diseases cause a special alarm due to high frequency and severity, as well as increased lethality rate (from 30 up to 75 %) over the last years (Goldstein et al., 2005; Wolfler et al., 2008) [5, 10]. At present time, even in the countries with high level of medical and social care for population the mean level of lethality from sepsis is 35 %, and in patients with septic shock achieves 60-70 % (Bon, 1991) [1]. Today the reasons of high lethality from sepsis in children require studying this problem more deeply, taking into account the current positions in the pathogenesis of this disease.
In recent literature (Bon, 1991; Chernyh et al., 2001; Goldstein et al., 2005; Michalek et al., 2007; Ren et al., 1999), there are new approaches for understanding sepsis pathogenesis, in basis of which underlies systemic inflammatory response syndrome (SIRS) that develops in response to bacterial aggression and is accompanied by emission of a plenty of inflammatory mediators into blood flow [1, 4, 5, 6, 8].
The start of cytokine cascade includes proinflammatory and antinflammatory cytokines. The balance between them is considered by Chernyh et al. (2001) to define the nature of clinical course and outcomes of purulent-septic diseases [4].
Despite several studies on nonspecific mediators of inflammation in the organism due to sepsis (Michalek et al., 2007; Rey et al., 2007), however, specific mediators of inflammation as lymphotoxins in this pathology are not well studied.
This study presents the results of investigation of specific proinflammatory lymphotoxins in early age children with sepsis and comparison of the data obtained with peculiarities of clinical course of disease.
The purpose of research was to study specific proinflammatory lymphotoxins in infants with sepsis.
Materials and methods of research
There were studied 33 infants with septicemic and septicopyemic forms of sepsis. Lymphocytes products - lymphotoxins to various microorganisms inducing sepsis were determined by author´s own method (Diagnosis of sepsis and evaluation of treatment efficacy, diploma № DG 400819). We developed a technique of isolation and identification of proinflammatory specific mediators of inflammation - specific lymphotoxins in infants with sepsis. The principle of this method concludes the measurement of specific toxicity to various antigens of liquid above the sediment which was received after cultivation of the patient´s lymphocytes with guilty antigens. The cultures of Staphylococcus aureus, E.Coli, clostridium, proteus, epidermic staphylococcus, preliminary isolated from children with sepsis were taken as antigens. To define the level of lymphotoxins isolated from sensibilized lymphocytes their calculation on spectrograph was used.
The diagnosis «sepsis» was made, based on summarized analyses of child´s condition, clinical symptoms of disease and laboratory examinations. Sepsis was confirmed by bacteriological study.
The samples from pharynx, blood, pus, urine and feces were investigated for presence of pathogenic flora. All patients received the standard treatments: antibiotics, specific therapy, symptomatic treatment, immunocorrecting therapy, eubiotics, phages.
Mathematic processing of the results obtained were performed with the use of method of variation statistic and calculation of mean arithmetic values (M), their standard errors (m), confidence interval (σ) and reliable differences according to Student´s t-criterion.
Results of research and their discussion
The results of this study showed specificity of lymphotoxin synthesis as the products which are activated by Т-lymphocyte antigens in infants with sepsis.
There were studied lymphotoxin products to Staphylococcus aureus, E.Coli, clostridia, proteus, epidermal staphylococcus with various forms of sepsis before treatment and in order to estimate the efficiency of the carried out therapy.
Studies showed that the highest values of lymphotoxin to Staphylococcus aureus were produced in septicemic form of sepsis (24,4 ± 0,9 optic units) (o.u.) (Fig. 1).
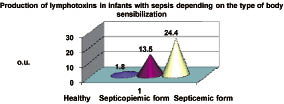
Fig. 1. Lymphotoxins to Staphylococcus aureus
This parameter was 1,7 times higher than values in septicopyemic form of sepsis (13,5 ± 0,8 о.u.) (р < 0.001). These parameters in two forms of sepsis were higher than in group of healthy children (1,8 ± 0,1 o.u.). The number of positive cases in septicopyemic form of sepsis accounted for 19 of 33 examined (57,5 %) children.
Lymphotoxin levels in various forms of sepsis correlated with severity of child´s condition. In dynamics of the therapy conducted, lymphotoxin levels decreased not in all cases (р > 0,05).
Lymphotoxin levels to proteus in septicemic form was 30,2 ± 2,3 о.u., whereas in septicopyemic form its values were lower and amounted 18,9 ± 1,9 о.u., respectively (p < 0,001) (Fig. 2). These values were almost in three times higher than parameters of healthy children (6,3 ± 0,8 о.u.; p < 0,001). Dynamic study showed insignificant decrease of this parameter (p > 0,05).
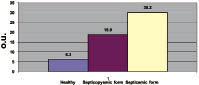
Fig. 2. Lymphotoxins to proteus
Production of lymphotoxins to E. Coli in healthy infants amounted 8,0 ± 1,1 о.u.
(Fig. 3). In 7 infants with septicemic form of sepsis the sensibilization of lymphocytes to E. Coli was 54,2 ± 3,7 o.u.; in 10 patients with septicopyemic form it was 29,5 ± 3,5 o.u., respectively. Sensibilization of lymphocytes to E. Coli was noted in 17 patients of all 33 studied and was 51,5 % of cases. After the treatment the sensibilization to E. Coli reduced 1.2 times (р < 0,05).
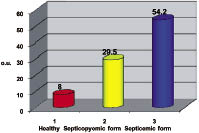
Fig. 3. Lymphotoxins to E.Coli
Production of lymphotoxins to epidermal staphylococcus in healthy infants was 10,4 ± 1,7 о.u. In 17 (56.7 %) of 30 examined patients there was noted sensibilization to epidermal staphylococcus (Fig. 4). The amount of lymphotoxins to epidermal staphylococcus was 30,8 ± 2,1 o.u. This parameter was 3 times higher than values in healthy children (p < 0,001). After the therapy performed the parameters of lymphotoxins to epidermal staphylococcus were reduced up to 22,4 ± 1,7 o.u., despite of decreasing the values were not reliable in comparison with parameters before treatment (p > 0.05).
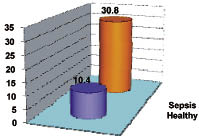
Fig. 4. Lymphotoxins to epidermic staphylococcus
The amount of lymphotoxins to clostridia in various forms of sepsis was 30,1 ± 4,0 o.u. before treatment that was 2 times higher than norm (p < 0,001) (Fig. 5). After treatment the values reduced up to the norm (p > 0,05).
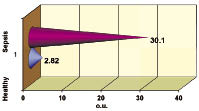
Fig. 5. Lymphotoxins to clostridium
For the patients with unchanged high values of lymphotoxins after therapy performed, we developed the further treatment program (continuing course of antibioticotherapy according to indications, bacteriophages and symptomatic therapy directed to the correction of polyorganic insufficiency) in order to prevent further recurrences of disease.
Production of specific lymphotoxins correlated with the positive bacteriological data confirming sepsis. In the negative values of lymphotoxins, bacteriological studies of blood, urine and feces were sterile in 100 % of cases.
Conclusions
Thus, the immune system of infants with various forms of sepsis directly reacts to antigenic irritation forms of cellular immune response that can be reflected in the clinical manifestations of disease. Dynamic studying of specific lymphotoxins levels during treatment showed incomplete correction of the immune disturbances, so in this case it is important to note a principle of an individual approach to the treatment of every patient depending on the character of pathogens revealed, phase and severity of pathological process, as well as immunity state.
References
- Bon R.C. The pathogenesis of sepsis // Ann. Int. Med. - 1991. - Vol. 115. - P. 457-469.
- Caresta E., Pierro A. et al. Oxidation of intravenous lipid in infants and children with systemic inflammatory response syndrome and sepsis // Pediatr. Res. - 2007. - Vol. 61 (2). - P. 228-232.
- Carvalho P.R., Feldens L. et al. Prevalence of systemic inflammatory syndromes at a tertiary pediatric intensive care unit // J. Pediatr. (Rio J). - 2005. - Vol. 81 (2). - P. 143-148.
- Chernyh U.R., Leplina O.J., Tikhonova M.A., Paltsev A.V., Ostanin А.В. Cytokine balance in the pathogenesis of systemic inflammatory response: a new target of immunotherapeutic influences for sepsis treatment // J. Med. Immunology, in Russian. -2001. - Vol. 3(3). - P. 415-429.
- Goldstein B., Giroir B., Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics // Pediatr. Crit. Care Med. - 2005. - Vol. 6 (1). - P. 2-8.
- Michalek J., Svetlikova P. et al. Interleukin-6 gene variants and the risk of sepsis development in children // Hum. Immunol. - 2007. - Vol. 68 (9). - P. 756-760.
- Pavare J., Grope I., Gardovska D. Prevalence of systemic inflammatory response syndrome (SIRS) in hospitalized children: a point prevalence study // BMC Pediatr. - 2009 - №9. - P. 25.
- Ren C., Liu X., Guo Z. et al. Syndrome of the systemic inflammatory answer in patients at intensive therapy department - analyses of 1292 cases // Zhonghua-Nci-Kc-Za-Zhi. - 1999. - Vol. 38 (1). - P. 40-43.
- Rey C., Los Arcos M., Concha A., Medina A., Prieto S., Martinez P., Prieto B. Procalcitonin and C-reactive protein as markers of systemic inflammatory response syndrome severity in critically ill children // Intensive Care Med. - 2007. - Vol. 33 (3). - P. 477-484.
- Wolfler A., Silvani P., Musicco M., Antonelli M., Salvo I. Incidence of and mortality due to sepsis, severe sepsis and septic shock in Italian Pediatric Intensive Care Units: a prospective national survey // Intensive Care Med. - 2008 - Vol. 34 (9). - P. 1690-1697.

