Introduction
Botulism is a rare, but potentially fatal, infectious disease caused by the neurotoxin produced by the anaerobic bacterium Clostridium botulinum bacterium [1, 2]. The disease damages the peripheral nervous system, leading to flaccid paralysis that requires immediate medical attention [3]. Despite advances in intensive care and mechanical ventilation, the mortality rate remains high, particularly in cases where the diagnosis is delayed and specific treatment is not available [4]. According to the World Health Organization (WHO), approximately 1,000 cases of botulism are reported annually worldwide, of which 5-10% are fatal [5].
The clinical presentation of botulism can vary from nonspecific gastrointestinal symptoms to severe neuromuscular complications, making early diagnosis challenging [6]. In recent years, there has been a decrease in the number of cases, but outbreaks related to the consumption of home-canned food continue to be reported [7].
According to the Ministry of Health and the Sanitary and Epidemiological Service of the Kyrgyz Republic, the number of botulism cases varies from year to year. In 2018, there were 93 cases, in 2019 – 46 cases, in 2020 – 68 cases, in 2021 – 81 cases, in 2022 – 41 cases, and in 2023 – 99, in 2024 – 78 cases. These numbers indicate the continued importance of the botulism problem in the country [8]. A systematic analysis of botulism cases and patient outcomes is crucial for improving timely diagnosis and preventing adverse outcomes.
This article analyzes family cases of foodborne botulism that arose in the Naryn region of the Kyrgyz Republic after consuming an industrially canned product. The clinical and epidemiological features of the disease, the influence of late diagnosis and errors in the initial diagnosis on the course of the disease are considered.
The purpose of the study was to analyze the epidemiological and clinical laboratory manifestations of botulism cases in the family home when using an industrial canned product.
Materials and methods of research
This work is a retrospective study of clinical and laboratory parameters of cases of food-borne botulism in a family home in the Naryn region of the Kyrgyz Republic. The study included 7 patients admitted to the Naryn Regional United Hospital from August 22 to September 4, 2024. The main clinical materials used were patient medical records and laboratory test results.
Results of the research and discussions
Among the observed patients, an extremely severe form of foodborne botulism was detected in one patient (14.2%), a severe form was also registered in 1 patient (14.2%), and the rest had moderate-severe forms of the disease in 5 (71.6%) (Fig. 1). It should be noted that there was 1 child among the observed patients.
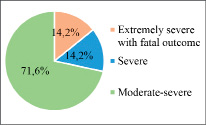
Fig. 1. The severity of botulism in the family hearth
It was found out from the epidemiological history that all the patients who applied (all family members) fell ill with botulism after consuming the Adjika product purchased in one of the supermarkets in the region.
In all patients, the main clinical symptoms were the following syndromes: intoxication, asthenovegetative and bulbar syndromes – 100%. Gastrointestinal symptoms and myoneuroplegia were found in 71.50% of cases. Ophthalmoplegic syndrome was noted in 85.70% of patients. Acute respiratory failure was registered in patients with severe and extremely severe forms -28.50% (Fig.2).
Below are two clinical cases of food-borne botulism, one in an elderly patient that ended in death and another in a child, with a severe course due to very late diagnosis of the disease and late management of anti-botulinum serum.
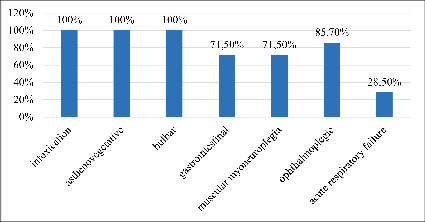
Fig 2. Clinical characteristics of botulism in the family home
The clinical example №1
Patient S.T., born in 1957, was in the Naryn Regional United Hospital (NRUH) from 08/22/2024 to 08/25/2024 with a clinical diagnosis of Botulism. Acute respiratory failure of the 3rd degree. Acute cardiovascular insufficiency. Hypertension of the 3rd degree, very high risk.
The patient was admitted on 08/22/2024 at 3.15 p.m. by ambulance with complaints of speech disorders, headache, pain when swallowing, and ptosis on both sides.
It was found out from the anamnesis of the disease that the man became acutely ill (08/21/24) when the patient had general weakness, pain when swallowing, and speech disorders.
Objectively, upon admission, the condition was assessed as severe. Body temperature is 36C. The skin is clean, there is no cyanosis. Eyes with no special features, hearing and smell without special features. The sensitivity of the skin is not impaired. Respiratory rate - 18 per minute. The pulse is 78 per minute. Blood pressure is 140/40 mmHg. Nervous system: consciousness is clear, the eye slits are the same, the pupils are rounded, the eyeballs move in full, the face is symmetrical. Notes dizziness. Swallowing is impaired. Tongue sticking out along the midline. Reflexes D = C. Muscle tone and strength are unchanged. Sensitivity is preserved. The functions of the pelvic organs are preserved. Meningeal symptoms are negative. The memory is saved. Dysarthria. The gait is not broken. Red dermographism. He is stable in the Romberg pose. Local status: semi-ptosis on both sides, dysphagia, pupils D=C, double vision, swallowing reflex decreased.
The neurologist diagnosed acute ischemic stroke. A medulla oblongata infarction? Bulbar syndrome? Exclude myasthenia gravis. And was he hospitalized in the Department of angioedema with a diagnosis of Ischemic stroke, bulbar syndrome?
08/23/2024, a second telephone consultation was conducted and a clinical diagnosis was made: Myasthenia gravis, generalized form. The patient’s general condition progressively worsened. And on 08/25/24, a consultation was held with an infectious disease specialist, a neurologist, and an intensive care specialist. It was only during the consultation that it was found out, according to the patient’s wife, that on 08/21/24, all family members consisting of 7 people consumed canned food “Adjika” bought at the supermarket during lunch. It was also found out that the same symptoms noted above were observed in the son, who left for Bishkek and was hospitalized at the Republican Clinical Infectious Diseases Hospital (RCIDH). Was my son clinically diagnosed with Botulism with damage to the cranial nerves at the RCIDH? And he was transferred to the intensive care unit.
08/23/2024, patient S.T. was transferred to the intensive care unit. He was conscious, but he was barely accessible to contact, and he answered questions indistinctly. Ophthalmoplegic symptoms and aphagia persisted. Respiratory rate is 23-24 per minute, pulse is 102-106 per minute, blood pressure is 177/109 mmHg. Laboratory data: hemogram without features, the results of biochemical analyses were within the normal range, coagulogram without pathology. Computed tomography of the brain dated 08/22/2024. Conclusion: no structural changes in the brain substance were detected. There are subdural hygromes on the convexital surface of the frontal and parietal lobes on both sides. The kimmerli anomaly is on both sides. The patient’s electrocardiogram was without any special features.
The anti-botulinum serum (one therapeutic dose) was administered only on 08/25/2024 at 16 o’clock, on the 4th day of the patient’s admission to the hospital and on the 5th day of the illness after the late verification of the clinical diagnosis (Botulism. Acute respiratory failure of the 3rd degree. Acute cardiovascular insufficiency).
Despite the fact that they administered anti-botulinum serum (one therapeutic dose), patient S.T. was diagnosed with biological death on 08/25/2024 at 19.20 hours.
The clinical example №2
Patient K.A., born in 2012, received inpatient treatment from 08/23/2024 to 09/04/2024 at the hospital in the infectious diseases department. Upon admission to the hospital, there were the following complaints: cough, weakness, fever. From the anamnesis of the disease: the disease began acutely with a cough, an increase in body temperature. Due to the deterioration of his condition, he was hospitalized in the NRUB infection department. It was found out from the epidemiological history that the child got sick after eating the Adjika product along with the rest of the family.
Objectively: the general condition is of moderate severity. Consciousness is inhibited. The position is forced (it is not described what is the reason), discharge from the nose on the right and left. Breathing above the lungs is hard. The breathing rate per minute, rhythm and type of breathing were not determined. There is no cyanosis. Heart rate – there is no record. The heart tones are preserved. Blood pressure is -100/80 mmHg. The mucous membranes of the oral cavity are pale, the tongue is coated. The abdomen is of normal size, the liver size is normal. The stool is regular. Urination is free. Neuropsychological system: Clear consciousness, neurological status- perceives well, the eye slits are the same, the pupils are rounded, the eye movement is in full, the face is symmetrical, there is no dizziness, swallowing is preserved, the tongue protrudes along the midline, superficial and deep reflexes are without features. Sensitivity is preserved, meningeal symptoms are negative. He is unstable in the Romberg pose. Local status: weakness, vomiting, cough.
Based on complaints and objective data, a preliminary diagnosis was made of “Enterovirus infection, severe course. Neurotoxicosis”.
The results of a general urinalysis from 08/24/2024 were within the normal range. The hemogram from 08/23/2024 showed leukocytosis (leukocytes 25.2*10^9/L), the remaining indicators were without pathological changes. Blood calcium – 2.67 mmol/L; sugar -3.74 mmol/L; Liver tests: total bilirubin – 9.9 mmol/L; direct bilirubin – 3.84 mmol/L; ALT – 11.2 units/L; AST – 19.3 units/l; amylase – 48.7 units/L; creatinine – 47.9 mmol/l; urea – 7.98 mmol/l; thymol sample -1.17 units; sodium – 137.1 mmol/l; total protein – 69.9 g/l; procalcitonin – 0.1 ng/ml.
08/25/2024, at 13:10 p.m., the child’s general condition deteriorates dramatically and is examined by an infectious disease specialist, pediatrician, pediatric neurologist, and pediatric intensive care specialist. As a result of the consultation, the main clinical diagnosis was not verified. However, due to the severity of the condition, the child is transferred to the intensive care unit.
The child’s condition is assessed as severe due to symptoms of intoxication. The mind is inhibited. He is reluctant to make contact. Hemodynamics is stable. Severe symptoms of intoxication and general weakness persist. He drinks poorly, and his appetite is reduced. The skin and visible mucous membranes are normally colored. The pharynx is vividly hyperemic, the tonsils are enlarged, covered with a purulent coating. The tongue is moist, covered with a white coating. Difficulty swallowing is noted, and the eyes are slightly sunken. Breathing is hard in the lungs, there is no wheezing. The heart tones are clear and rhythmic. The belly is soft. Stools and diuresis are regular.
08/25/2024 (15:00), the patient’s condition was severe, her temperature was 36.7, and her blood oxygen concentration was 86%. Severe weakness and swallowing disorders persist. Shortness of breath and weakness. There is no respiratory failure. Hemodynamics is stable. He drinks the liquid badly. The skin and visible mucous membranes are normally colored. The eyes are slightly sunken. The pharynx is vividly hyperemic, the tonsils are enlarged, covered with a purulent coating. Lips are dry. The tongue is covered with a white coating. Breathing is hard, there is no wheezing. Heart tones without features. Detoxification, antibacterial and infusion therapy were included in the treatment.
08/25/2024 (18:00) symptoms of intoxication persist, body temperature is 36.7, pulse is 98 beats per minute, oxygen concentration in the blood is 96%. The neurological symptoms are the same. Biotonics is difficult. There is no respiratory failure. He drinks the liquid with difficulty. The objective status remains the same. There is no stool, urinate on your own.
08/25/2024 (21:00) at the time of the examination in the evening, the general condition did not deteriorate. Hemodynamics is stable. Conscious, sleeping a physiological sleep. Breathing is not difficult. Appetite is reduced. Body temperature is 36.7, pulse is 101 beats per minute, oxygen concentration in the blood is 97%. The other parameters of the objective status are the same.
08/26/2024 (09:30) in the morning, a second consultation was held with the participation of a pediatric infectious diseases specialist, a pediatrician, a pediatric neurologist, and a pediatric intensive care unit, and the final clinical diagnosis was made: Botulism. Severe form. And an anti-botulinum serum of type A. At 17:00, type B and E serum was administered (1.8 ml i/m). Ciprofloxacin 100 ml IV x2 times a day, neuromidin 1.5%-1.0 i/m, mixers – 4 ml i/m are additionally prescribed for treatment. At 08/29/24, it was decided to re-administer the anti-botulinum serum.
08/31/2024, a positive trend was noted in the child’s general condition. Patient started walking with the help of the support of the medical staff, but she quickly got tired. Feeding remained through the probe. The eyelids were lifting. The stool is normal and the diuresis is regular.
09/02/2024 due to the positive dynamics and stable general condition, the child was transferred from the intensive care unit to the infectious diseases department.
09/03/2024 (08:00) in the morning after the third doctors’ consultation, the child was discharged home in satisfactory condition with a final clinical diagnosis: Food-borne botulism, severe form. Acute pharyngotonsillitis. Candidiasis of the pharynx and oral cavity. Bilateral ethmoiditis. A cyst of the maxillary sinus on the left.
The remaining 5 patients from this family had a moderate-severe form of botulism, despite the late diagnosis and administration of anti-botulinum serum. All these patients were discharged from the hospital in a satisfactory condition.
Conclusions
A clinical and epidemiological study of cases of foodborne botulism in one family affected by the consumption of the industrial product “Adjika” revealed the characteristic features of the course, diagnosis and outcomes of the disease.
1. In all cases, the source of botulinum intoxication was the same industrial product, which underlines the urgency of strict food quality control at all stages of production and sale.
2. Intoxication, asthenovegetative and bulbar syndromes dominated in all patients (100%). The most common manifestations were ophthalmoplegic syndrome (85.7%) and gastrointestinal symptoms with myoneuroplegia (71.5%). Acute respiratory failure developed in patients with severe and extremely severe course (28.5%).
3. In both severe clinical cases (in an adult patient with a fatal outcome and in a child), the diagnosis of botulism was established late, which led to untimely administration of anti-botulinum serum and a worsening of the prognosis. Initially, erroneous diagnoses were made (ischemic stroke, myasthenia gravis, enterovirus infection), which demonstrates the need to increase the alertness of doctors of all specialties regarding botulism in the presence of a characteristic history and symptom complex.
4. Death was recorded in one elderly patient (14.2%), which is associated with late diagnosis and administration of serum on the 5th day of the disease. The child with severe form recovered after combination therapy, including administration of multivalent anti-botulinum serum and intensive infusion, antibacterial therapy.
5. Laboratory tests were not fully performed for all patients, as this region is located in the highlands very far from the central part of the region, and therefore many tests were unavailable.
6. The positive outcome in the majority of patients with moderate-severe forms, despite the late diagnosis, underlines the effectiveness of timely detoxification therapy and the use of serum even in the late stages of the disease.
Thus, the results of the study confirm the critical role of early diagnosis, detailed epidemiological history and immediate administration of a specific serum in the prognosis of botulism. The data obtained can serve as a basis for the development of regional clinical protocols and algorithms for the management of botulism patients, especially in case of group outbreaks.

