Introduction
Diabetes mellitus (DM) belongs to the category of socially significant non–communicable diseases with epidemic rates of increase in prevalence. According to the Federal Register of Statistics of the Russian Federation, the prevalence of type 2 diabetes in the Russian Federation on average at the beginning of 2023 was 3158.8/100 thousand of the population [1]. The incidence is growing not only in Russia, but also around the world. According to the IDF Diabetis Atlas, the number of diabetic patients in 2021 is 536 million people aged 20 to 79 years, and the expected increase by 2030 is 106 million people [2]. Diabetes mellitus disrupts the function of all organ systems 3.8 million people die from complications of this disease every year. In patients with diabetes mellitus, mortality from heart disease and stroke is 2-3 times higher, blindness is approximately 10 times more common, nephropathy is 12-15 times higher, gangrene of the lower extremities is almost 20 times higher than in the general population [3].
The aim of the study was to analyze medical histories of patients to assess the nature of the course of comorbid pathology, that will contribute to the early detection of diseases and the prevention of complications.
Materials and methods of research
As the materials were taken 59 case histories of patients treated in the day patient department of the Voronezh State Out-Patient Clinic No.4. Of these, 36 were women and 23 were men. Enrolment criteria was comorbidity involving type 2 diabetes mellitus (DM2) and coronary heart disease (CHD). We analyzed associated diseases in this group of patients. According to WHO criteria, the age of patients ranged from average to senile, while three age groups were identified: middle-aged group (45-59 years), elderly age group (60-74 years) and a senile age (75-90 years). The selection criteria were the presence of a history of comorbidity of type 2 diabetes mellitus and coronary heart disease. The presence of concomitant diseases was assessed in the medical records.
Early glycemic disorders, such as impaired glucose tolerance and fasting glycaemia, precede the development of DM2. This condition is called prediabetic, the number of people with impaired glycemia significantly exceeds the number of patients with DM2. As it progresses, prediabetes significantly increases the risk of developing heart disease, and can also turn into DM2 [4].
DM2 is a chronic disease characterized by the disruption of normal carbohydrate metabolism primarily due to insulin resistance and relative insulin deficiency. Alternatively, it may be caused predominantly by an impairment in insulin secretion, either independently or concurrently with varying levels of insulin resistance.
In many cases DM2 characterized by insulin resistance of tissues, in response to which compensatory hyperinsulinemia occurs, as well as chronic hyperglycemia and dyslipidemia. All of these factors have a damaging effect on the vascular system, as a result of a chronic inflammatory process. Vascular damage leads to the development of multisystemic pathology, especially affecting the cardiovascular system. According to the results of causes of death in the presence of DM2 for 2010-2022, the largest percentage was congestive heart failure- 24.2%, followed by atherosclerotic cardiovascular diseases, which include coronary heart disease and myocardial infarction (MI), cerebral circulation disorders and acute cardiovascular events [5].
DM2 leads to damage to vessels of both small and large caliber, coronary vessels often suffer, leading to the development of coronary heart disease. A statistical analysis of patients from all over the world in 2007-2017 showed that 21.2% of patients with DM2 have coronary heart disease [6].
According to a study conducted by Sarwar and co-authors, which involved more than 450,000 people, diabetes increases the risk of coronary heart disease by about two times in men and three times in women [7].
It was also noted that in DM2, there was a myocardial infarction in 3.7% of cases [5].
Coronary heart disease and DM2 have common links in pathogenesis. The leading pathogenetic factor is hyperglycemia, which is accompanied by oxidative stress. With hyperglycemia, an excessive amount of glucose accumulates in endothelial cells, which is supplied by simple diffusion. Glucose and its metabolites damage plasma proteins and blood cells, as well as glycate proteins of the vascular endothelium. Along with this, malondialdehyde accumulates as a result of lipid peroxidation. A key role in this process is assigned to reactive oxygen species (ROS), which is associated with mitochondrial dysfunction. In mitochondria, ROS synthesis occurs in the electron transport chain due to nutrient overload, namely glucose, which leads to excessive production of a superoxide radical, the level of which is not compensated by conventional antioxidant mechanisms.
Excess glucose in the body tissues triggers the process of its metabolism along the polyol pathway. As a result of the accumulation of by-products of this process, the production of ROS by the mitochondria of cells increases, which leads to the progression of oxidative stress.
Excessive oxidation of glucose and glycerol leads to an increase in the intracellular concentration of diacylglyceride, which affects the expression of genes responsible for the production of protein kinase C. This type of kinase stimulates the production of NADP oxidase, phospholipase A2, endothelin-1 and endothelial growth factor, which leads to vascular spasm, division of smooth muscle cells and activation of extracellular matrix protein synthesis [8].
A study by Poznyak and co-authors shows the effect of diabetes on the risk of cardiovascular disease in patients with dyslipidemia. It was revealed that the chronic intravascular inflammatory process contributes to the progression of atherosclerosis and vascular obstruction as a result of dyslipidemia. Oxidative stress leads to the activation of adhesion molecules on the surface of the endothelium, which leads to the migration of macrophages into the forming atherosclerosis plaque. Constantly elevated glucose levels induce protein glycation. The end products of their metabolism accumulate in patients with DM2 with elevated blood glucose levels and provoke atherosclerosis. These molecules affect the activation of the endothelium and the surface expression of adhesion molecules, thereby promoting adhesion and entry of macrophages into the subendothelial space at the initial stages of plaque formation, the presence of macrophages stimulates the inflammatory process inside the atherosclerotic plaque [4,9].
Small atherogenic very-low-density lipoproteins penetrate the damaged vessel wall and are phagocytized by immune cells and they turn into foam cells. they ferment all the components of lipoproteins except cholesterol. Dyslipidemia in DM2 is characterized by a predominant increase in triglycerides. Insulin resistance activates hormone-sensitive lipase in adipose tissue, which increases the amount of free fatty acids and increases the production of hepatic triglycerides. Insulin resistance also stimulates the production of atherogenic VLDL in the liver [9].
DM2 contributes to the formation of atherogenic modifications of LDL, they are the main sources of cholesterol for atherosclerotic plaques. Low-density lipoproteins are desialyzed in the blood, as a result they acquire a negative charge, become denser and decrease in size. At the same time, the synthesis of HDL in the liver, which have an antiatherogenic effect, decreases [10].
Constantly elevated glucose levels induce protein glycation. The end products of their metabolism accumulate in patients with DM2 with elevated blood glucose levels and provoke atherosclerosis. These molecules affect the activation of the endothelium and the surface expression of adhesion molecules, thereby promoting adhesion and entry of macrophages into the subendothelial space at the initial stages of plaque formation, the presence of macrophages stimulates the inflammatory process inside the atherosclerotic plaque [11].
Patients with DM2 are characterized by a decrease in the activity of the fibrinolytic system, which increases the risk of thrombosis. The main factors contributing to hypercoagulation in DM2 are platelet activation, endothelial cell dysfunction (EC), increased thrombin production, proinflammatory state, increased fibrinogen levels along with its modifications, as well as changes in the structure of fibrin. Obesity, which often accompanies DM2, hyperinsulinemia and hyperglycemia, lead to platelet activation, which is reflected in the increased release of thromboxane A2, P-selectin, plasminogen-1 activator inhibitor and platelet microparticles. Another factor contributing to platelet activation is oxidative stress. ROS are activated by the end products of glycation, which leads to the activation of a tissue factor that triggers an external cascade of coagulation-plasma hemostasis reactions [12].
In DM2, the diagnosis of coronary heart disease is complicated by the painless course of this disease, coronary heart disease may be accompanied by nonspecific symptoms (weakness, attacks of suffocation, arrhythmia). Diabetic autonomic cardiovascular neuropathy and myocardial sympathectomy lead to such manifestations, i.e. vegetative and pain sensitivity is impaired. Due to the decrease in sensitivity, diabetics may not feel severe, burning chest pain with irradiation during angina attacks, and in some cases they may not even realize that they have a myocardial infarction. The cause of this phenomenon is considered to be cardiovascular autonomic neuropathy.
Hyperglycemia and the accompanying oxidative stress in nerve fibers lead to damage to the microvascular endothelium in the capillary networks of neurons of the autonomic nervous system.
The end products of glycation damage microvessels, blood-supplying neurons, and ischemia and apoptosis of nerve tissue cells develop. It has also been revealed that inflammatory mediators such as C-reactive protein, interleukin-6 and tumor necrosis factor-α contribute to nerve damage. Damage to the nervus vagus, which provides parasympathetic innervation of the heart, leads to a predominance of sympathetic influences on the regulation of the heart. Under the influence of sympathies, tachycardia and an increase in blood pressure occur, the load on the heart increases and cardiomyopathy progresses [13].
In type 2 diabetes mellitus, atherosclerotic changes and increased thrombosis in blood vessels lead to disorders in the microcirculatory system and an increase in total peripheral resistance. initially, the heart reacts with hypertrophy, the myocardial oxygen demand increases. narrowed coronary vessels cannot provide adequate oxygen transport, and therefore coronary heart disease progresses and the risk of myocardial infarction increases [13,14].
Myocardial infarction with DM-2 is 3 times more common, compared with patients without impaired carbohydrate metabolism, it is more severe, increasing the risk of complications. Studies confirm that with dm2, the frequency of repeated myocardial infarctions with complications in arrhythmia, cardiogenic shock, and cardiac tamponade is higher. The reasons for myocardial infarction include an increase in blood clotting and a decrease in the fibrinolytic ability of the blood, which eventually leads to the formation of blood clots.
The development of acute coronary syndrome exacerbates hyperglycemia by increasing the level of vasoactive cytokines, which can increase myocardial infarction and reduce insulin secretion. As a result, glucose utilization from the blood decreases, its intracellular concentration decreases, and metabolism shifts towards fatty acids, which leads to an increase in myocardial oxygen demand and increased hypoxia. These processes can lead to cardiogenic shock and the development of arrhythmia [14].
In the post-infarction period, there is a high mortality rate, in the first year after myocardial infarction – 15-34%, and over the next 5 years – 45%. Such indicators are associated with recurrent myocardial ischemia and, as a result, a slowdown in the formation of a connective tissue scar and the development of repeated heart attacks, the formation of heart failure [14].
Результаты исследования и их обсуждение
When analyzing the data, it was found that 88% of women and 43% of men of all age groups had angina pectoris, MI in 12% and 57%, respectively. In older men, the prevalence of MI is higher compared to women of the same age group. It was also noted that that coronary vascular revascularization by stenting or coronary artery bypass grafting was performed more often among men (63%) (fig. 1).
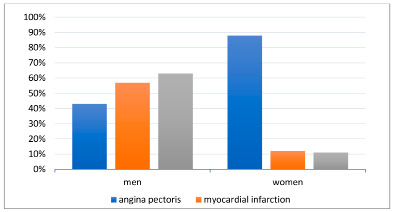
Fig.1.The incidence of angina pectoris, myocardial infarction and stenting among patients with comorbid pathology (DM2+CHD)
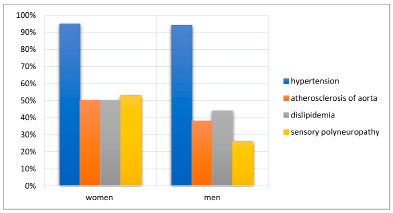
Fig.2.The incidence of concomitant diseases among patients with comorbid pathology (DM2+CHD)
In old age, 39% of women and 50% of men had second-degree obesity, third-degree obesity in 33% and 25%, respectively.
Of the concomitant diseases among elderly women, hypertension was the most common-95%, sensory polyneuropathy in 53% of cases, atherosclerosis of aorta and dyslipidemia occurred in 50% of cases. Hypertension was also the most common in men-94%, atherosclerosis of aorta was found in 38%, dyslipidemia in 44%, sensory polyneuropathy accounted for 26% of cases (fig. 2).
There were also cases of joint diagnosis of coronary heart disease and DM2: among elderly women -22%, among elderly men 31%.
Conclusions
The conducted research allows us to draw the following conclusions:
1. The prevalence of coronary heart disease in DM2:
• Coronary heart disease in type 2 diabetes mellitus is more common in women than in men.
2. Severity of course and complications:
• In men with DM2 and coronary heart disease, comorbid pathology is much more severe than in women.
• Men with DM2 and coronary heart disease are more likely to develop myocardial infarction.
• Men with DM2 and coronary artery disease are more likely to require coronary artery revascularization surgery.
3. The risk of developing MI:
• The male sex increases the risk of developing myocardial infarction by almost 5 times.
4. Concomitant diseases in coronary heart disease and DM2:
• The most common concomitant diseases in the comorbidity of coronary heart disease and DM2 are arterial hypertension, sensory polyneuropathy, fatness, atherosclerosis of the aorta, dyslipidemia
5. Gender differences in concomitant diseases:
• All concomitant diseases have approximately the same percentage in men and women with DM2 and coronary artery disease.
• Sensory polyneuropathy is 2 times more common in women with DM2 and coronary heart disease than in men.
These findings highlight the importance of taking into account gender differences in the diagnosis and treatment of patients with DM2 and coronary artery disease. Men with DM2 require closer monitoring and early prevention of cardiovascular complications.
Further research is needed to clarify the mechanisms underlying gender differences in the course of comorbid diseases.

