Introduction
Despite medical advances, acute intestinal infections continue to be a significant public health problem. Whereas earlier acute intestinal infections were caused mainly by bacterial agents, in particular Salmonella, Shigella, E. coli, Klebsiella spp., Proteus spp., Enterobacter, Citrobacter spp. and others, today the leading role in the structure of acute intestinal infections morbidity is played by secretory diarrhoea of viral nature, namely by rotavirus, noro-, astro-, adeno-, sapovirus [1, 2]. Analysing the literature data, it was found that among viral diarrhoeas rotavirus infection prevails, and the second most important causative agents of acute gastroenteritis are noroviruses (NV), the role of which in sporadic incidence of acute gastroenteritis was significantly underestimated until recently [3, 4]. The circulation of noroviruses has increased dramatically since the mid-1990s. Epidemiological features of norovirus infection are prolonged excretion of the pathogen from the organism of patients and virus carriers, especially in immunosuppressed persons; implementation of various routes of transmission (food, water, contact and household, aerosol), high contagiousness. Sometimes outbreak, group and sporadic morbidity of norovirus gastroenteritis is registered. Outbreaks of norovirus infection (NVI) began to be recorded in educational institutions, kindergartens, catering facilities, tourist groups, cruise ships, etc., and they covered a significant number of people. In the world, 267 million cases of norovirus infection are registered annually, more than 1 million, about 200 thousand children under 5 years of age are hospitalised and die from norovirus gastroenteritis. In European countries from 1 to 20 million people fall ill annually. In Russia, noroviruses account for 5 to 27% of the etiological structure of acute intestinal infections [5, 6, 7]. According to European epidemiological studies, outbreak rates represent only the tip of the iceberg: only 1 out of every 1,562 cases is registered. The first localised outbreak of norovirus gastroenteritis in Luhansk was registered in April 2018 at secondary school № 17, with further occurrence of intra-family outbreaks. Norovirus gastroenteritis in children also manifested in 60% of cases in the form of gastroenteritis syndrome and in 40% – in the form of acute gastritis combined with pronounced general toxic symptoms. According to the results of the epidemiological investigation of the 2018 outbreak, the specialists of the city sanitary service found that all students drank boiled water from one kettle in the school canteen with an insufficient number of disposable glasses (a real possibility of infection through shared glasses). In addition, the school constantly lacked water from the centralised water supply system during the daytime (water shutdown in the city due to the emergency situation), which had an unsatisfactory effect on compliance with hygienic and anti-epidemic regimes. This made it possible to establish that the probable cause of norovirus infection in school № 17 was the contact and domestic route of transmission, mediated through infected glasses with drinking water and contaminated surfaces of various school items with pathogens of highly contagious intestinal viral infection. Subsequently, three more localised outbreaks in children’s educational institutions were registered in the territory of the Luhansk People’s Republic, the last of which is presented as a clinical case.
The aim of the study was to analyse the outbreak morbidity, determine the epidemiological, clinical and laboratory features of norovirus infection in children and adolescents in the Luhansk People’s Republic.
Material and methods of research
The study was conducted on the basis of the infectious disease department of the State budgetary health care institution «Alchevsk Central City Multidisciplinary Hospital», Luhansk People’s Republic. There were 32 adolescents (students of the cadet corps) aged 12 – 17 years, who were admitted from 23.05.24 to 29.05.2024 with a preliminary diagnosis of acute intestinal infections. All children underwent a set of general laboratory investigations. The diagnosis of norovirus gastroenteritis was made on the basis of epidemiological anamnesis (group morbidity, stay in the focus of infection, contact with patients), clinical data (signs of gastrointestinal tract damage, dehydration, intoxication) and laboratory data. Clinical observation was supplemented by common laboratory methods of examination: general blood analysis; general urine analysis; coprogram; stool analysis for worm eggs and protozoa. In single cases, additional investigations were performed as indicated: ultrasound of abdominal cavity organs, electrocardiography.
To establish the etiologic factor, a bacteriological examination of feces was used for the presence of salmonella, shigella, E. coli and opportunistic microflora (Klebsiella spp., Proteus spp., Enterobacter, Citrobacter spp.). Feces were examined for roto-, astro- and adenoviruses using a rapid test and latex agglutination reaction (LAR), and an immunochromatographic method (ICM). To detect norovirus RNA (norovirus genotype II RNA (Norovirus GtII)) feces were examined using the PCR method. All studies were performed on the 1st-3rd day after the patient’s admission to the hospital. During the observation, the general condition of the children, psychoemotional state (sleep, activity, reaction to a doctor’s examination, etc.), appetite, clinical and laboratory test data were assessed daily, and anamnesis was collected. When considering the clinical course of the disease, the authors of the article studied in detail its onset and course: duration of hospital stay, duration of intoxication, terms of normalisation of body temperature, terms of appetite recovery, dynamics of cessation of vomiting and diarrhoea, abdominal pain, flatulence, intestinal spasm, rumbling along its course and other manifestations of acute intestinal infection.
Results of the research and discussions
According to the aim, the authors of the article analysed the features of clinical symptomatology of norovirus infection in adolescent children.
The age structure of children was distributed as follows: 25% of the total number of hospitalised patients were 12-year-old children (8 people), 22% were 13-year-old children (7 people), 16% were 14-year-old children (5 people), 12% were 15-year-old children (4 people), 16% were 16-year-old children (5 people), and 9% were 17-year-old children (3 people) (Fig. 1).
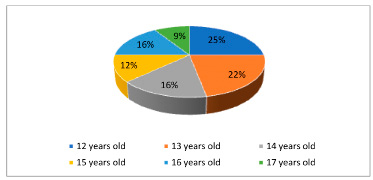
Fig. 1. Age structure of hospitalised patients
The clinical manifestation of norovirus infection in the presented cohort of children was characterised by the unification of intoxication, catarrhal and gastrointestinal syndromes. All patients with norovirus infection had acute gastroenteritis. All patients under observation were admitted for inpatient treatment within the first 12-48 hours after the onset of the initial clinical manifestations of the disease.
The severity of the condition was assessed from the moment of admission to the hospital, thus, the average degree of severity was established in 10 people (31,25%), in 20 people (62,5%) the condition was assessed as mild, carriage of norovirus infection was determined in 1 child (3,125%), contact with norovirus infection also took place in 1 adolescent (3,125%). In 93,75% of patients the beginning of the disease was acute, accompanied by fever, vomiting, diarrhoea and abdominal pain.
The intoxication syndrome was accompanied by lethargy in all the patients studied, pallor of the skin was determined in 5 children, decreased appetite – in 10. Fever syndrome was registered in 27 children (84,4%): in 31,3% of cases (10 people) there was a subfebrile temperature (from 37,2ºC to 38ºC), in 17 patients (53,1%) the temperature was in the range of 38,5ºC – 38,8ºC, at that, fluctuated up to 2 days. Catarrhal manifestations were insignificant in all age groups and were registered in 3 patients in the form of hyperaemia of the pharyngeal mucosa.
Damage of gastrointestinal tract was manifested by a number of symptoms: vomiting, abdominal pain, flatulence and liquid stools. The symptom of vomiting was quite characteristic, which was determined in 93,75% of cases, in 19 (59,37%) – multiple (5-10 times a day), in 11 children (34,38%) – single vomiting. Vomiting was predominant in 22 (68,75%) children and only 8 children (25%) had both vomiting and diarrhoea at the beginning of the disease. All children had contraction-like abdominal pain with localisation in the epigastrium and perineal region. On palpation of the abdomen, there was a diffuse painfulness along the course of the intestine. The pain syndrome lasted up to 2-3 days. Diarrhoea was observed in 19 children (59,4%) in hospital. The frequency of defecation ranged from 1 to 5 times, watery stools prevailed, less often liquefied or liquid, brown in colour, not abundant, without pathological impurities (Fig. 2).
Thorough collection of epidemiological anamnesis made it possible to establish: all children live in a dormitory. They eat in an organised manner in the canteen of the cadet corps. They use bottled water. In the course of epidemiological investigation it was established that a female employee of the cadet corps’ canteen carried norovirus and was the source of infection. Transmission factors could be a variety of foods that are not heat-treated.
Laboratory examination of all hospitalised patients revealed insignificant pathological changes, which were not of key importance in the diagnosis, but were auxiliary: leukocytosis (10-15 *10 9\l) with neutrophilic shift – in 17 (53,1%) patients, normocytosis with alkaline-nuclear shift, relative lymphopenia – in 6 (18,75%) patients; in other children the changes were insignificant or all parameters were within the normal range. Coprocytogram: in 13 children (40,6%) – presence of mucus and leucocytes – from 30 to the whole field of vision), which coincides with clinical manifestations – presence of intestinal dysfunction in these children (probability of enterocolitis).
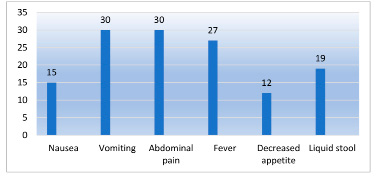
Fig. 2. Clinical picture in hospitalised patients
Stool tests for roto-, astro- and adenoviruses were negative. Bacteriological tests of stool for a group of acute intestinal infections were also negative. The diagnosis was verified in 32 cadets (100%) – RNA of norovirus genotype II (Norovirus GtII) was detected.
Based on the acute onset of the disease, pronounced intoxication syndrome (fever, lethargy, weakness, adynamia, drowsiness, refusal to eat) combined with abdominal syndrome (abdominal pain, repeated vomiting, nausea, in some cases diarrhoea), epidanamnesis (simultaneous group morbidity of intestinal infection in the cadet corps, specific laboratory tests of faeces for pathogens) was made the diagnosis «Acute gastroenteritis of norovirus etiology, medium severity», according to ICD10 – A08. 1 – acute gastroenteropathy caused by Norwalk pathogen.
Therapeutic measures were carried out in accordance with the prescriptions of the clinical recommendations of the Russian Federation on the diagnosis and treatment of norovirus gastroenteritis in children and included: dietary therapy table #4, oral rehydration using low-osmolar solutions (adiarin rehydrocomplex), enterosorbents (mineral, silicon-containing), probiotics containing Lactobacillus GG, Lactobacillus reuteri, Lactobacillus acidophilus, enzymes (pancreatin), antispasmodics. Infusion therapy was administered to 20 children (62.5%) with the purpose of detoxification and rehydration (exicosis of the first degree) [8].
On the 3rd day in hospital, the condition of the children was noted as stable, with a tendency to improvement – body temperature normalised, appetite improved, but abdominal syndrome, fatigue in the second half of the day, drowsiness remained pronounced. The children were discharged on the 6th-7th day of treatment in almost satisfactory condition. Control stool examination for norovirus RNA was negative.
Conclusions
1. Localised outbreaks of norovirus infection among students of children’s educational institutions in the territory of the Luhansk People’s Republic have been registered for the first time in the last few years. The true number of children sick with norovirus gastroenteritis in both the first and second cases was not established (‘iceberg phenomenon’).
2. The most likely route of transmission is food and household contact, due to the detection of norovirus carriage in the catering staff. There is contamination of food, water and cutlery with norovirus.
3. In clinical terms, norovirus gastroenteritis in children manifested both gastroenteritis and gastritis syndromes in combination with pronounced general toxic phenomena. Hypovolaemic and other complications were not observed.
4. Taking into account the intensification of norovirus infection spread, primarily among children, deterioration of living conditions in the Donbass region due to the emergency (military) situation, it is possible to forecast further increase in the level of norovirus infection morbidity, occurrence of local outbreaks among children and adults.
5. In any outbreak of acute intestinal infections, especially those occurring in children’s organised groups, patients should be examined for viral etiology (including the entire spectrum of known viruses), which will optimise not only the treatment of patients but also anti-epidemic measures.
6. In the focus of group morbidity of norovirus infection it is allowed to establish the diagnosis in a part of victims on the basis of clinical and epidemiological history without laboratory confirmation.

