In the structure of gynecological diseases the first place is occupied by inflammatory processes of the genital organs. The prevalence rate of chronic endometritis is in a wide range: from 0.2 % to 70 % [4, 14]. At the same time, in the population of women of reproductive age, uterine myoma are increasingly diagnosed, the proportion of which varies from 20 to 70 % [3, 18]. Identification of benign tumors of the uterus usually moves into the background its combination with chronic endometritis, even when there is indication of inflammatory processes of the genitals, which contributes to the limitation of the scope of examination of women under the existing standards.
It is known that in chronic endometritis there are no typical clinical manifestations of the disease. And the main clinical symptoms of uterine myoma, in the form of abnormal uterine bleeding, pelvic pain, anemia, frequent urination and dyspareunia, have a significant impact on the health and quality of life of women [8, 11].
Currently, the priority in the organ-preserving treatment of uterine fibroids belongs to hormone therapy, used as a neo – and adjuvant, and self-treatment options. At the disposal of the doctor today there is a huge selection of drugs for conservative therapy of uterine myoma – progestagens, gonadotropin-releasing hormone agonists, antagonists gonadotropin-releasing hormone, progesterone receptor modulators (antigestagens), as well as selective progesterone receptor modulator [10]. However, it should be recognized that in some cases, when taking hormonal drugs, side effects and complications occur in the form of pain or hemorrhagic syndromes, the frequency of which is insufficiently covered in the scientific and medical literature [1, 10]. The appearance of adverse events poses a problem for the doctor and the patient to choose further tactics of treatment: to continue conservative treatment or to lean in favor of surgery. According to the national and foreign literature, hysterectomy, as a method of treatment of uterine myoma, remains the most common operation in gynecologists around the world. The frequency of surgical interventions for uterine tumor is 50-70 %, of which the proportion of radical operations is 60,9-95,5 % [7, 15, 16].
Objective: to study the features of the local immune status and morphological picture of the endometrium in the event of complications of hormone therapy of uterine myoma.
Material and methods of research
A comprehensive examination of 157 women with uterine myoma, the size of which did not exceed 12-week pregnancy, mainly with intramural and subserotic localization of nodes, and with indications for conservative treatment. In group 1 (n = 112), complications in the form of hemorrhagic syndrome have been noted when taking hormonal drugs. In group 2 (n = 45) – complications of hormone therapy have not been recorded for 3 months. The control group (n = 31) consisted of healthy women. All patients underwent standard clinical and laboratory examination and complex ultrasound examination (ultrasound) with dopplerometry on the device “Logiq S8” from the company GE Healthcare (USA). Local immunity was assessed by interleukin content (IL-1β, IL-4) and tumor necrosis factor (TNF-α) in uterine aspirates. The study has been carried out by solid-phase immunoassay, according to the Protocol of the manufacturer, using a set of reagents Vector-BEST Novosibirsk. In group 1, endometrial biopsy was performed during hysteroscopy for subsequent morphological examination. Statistical processing of the study results was carried out using STATISTICA 7.0, SPSS 17 packages, as well as MS Excel’2003 statistical functions, with the derivation of m+m, percent, logarithmic means (x) with 95 % confidence interval and the reliability of differences (P) by student’s criterion.
Results of research and their discussion
The average age of the women in the study group has been 30.5 ± 4.3 years, in the comparison group – 30.2 ± 3.7 years, in the control group-30.2 ± 5.5 years, indicating the comparability of the groups for further study. The analysis of anamnestic data has shown that only half of the patients with uterine myoma at the time of data collection were able to realize their reproductive function, which had significant differences in comparison with the control group (fig. 1).
The early onset of sexual activity has been noted by 51.8 % of group 1 patients, which was 8 times higher than the control group indicator (6.5 %) and almost 2 times – the same parameter of group 2 (26.7 %). The proportion of infertility and spontaneous abortions in women with complications of hormone therapy of uterine myoma was also significantly higher (1.3-1.4 times) than in group 2 (fig. 1). Among gynecological diseases in group 1 prevailed colpitis, chronic inflammation of the pelvic organs and benign diseases of the cervix, the frequency of which significantly exceeded the similar parameters of group 2 and the control group. According to the modern literature, the transferred inflammatory diseases of genitals and urogenital infections should be referred to the risk factors of uterine tumor [7, 11, 13].
According to our data, ovarian-menstrual cycle disorders have been registered more frequently in patients of groups 1 and 2 compared to control data. And the use of intrauterine devices in history for contraception has been observed only in the groups of women with uterine myoma, and the obtained value in group 1 have been 5 times higher than in group 2.
The variants of conservative therapy of uterine fibroids in the groups have been characterized by a variety of hormonal drugs (fig. 2).
In group 1 there followed the randomness of the choice of means for the treatment of uterine myoma. In almost every third patient in this group, combined oral contraceptives (COC) have been used, which have never been mentioned in group 2. In every fourth case, gestagens (dufaston or “Mirena” intrauterine system) have been assigned to group 1. The frequency of Duphastone and the intrauterine system “Mirena” in group 1, respectively, 2.3 and 2.5 times higher than in group 2. Significantly less in the group of women with complications of hormone therapy for uterine myoma appointment of GnRH agonists (a-GnRH), mifepristone (Ginestre) and ulipristal acetate (ASME) (fig. 2) have been recorded. It should also be noted that 86.7 % of patients (n = 39) underwent antibacterial/ antiviral and immunomodulatory therapy in group 2 before taking hormonal drugs. In group 1, only 35 women (31.3 %) indicated for preliminary empirical treatment, with the inclusion of antibacterial agents, which was almost 3 times lower than the same indicator in group 2.
The results of complex ultrasound examination showed a significant increase in the average volume of the uterus in patients of groups 1 and 2 in relation to similar parameters of the control group (table 1).
Localization of the tumor of the uterus in 1 and 2 groups has been visualized predominantly interstitial, rarely subserous fibroids. The number of nodes varied from 3 to 6, and the size – from 1.5 to 3.6 cm.in the study of uterine hemodynamics in patients with uterine myoma, we did not reveal significant differences in the parameters of independent right and left uterine arteries. Therefore, for further research we used the average values of the velocity of systolic blood flow (V max), diastolic blood flow (V min) and resistance index (IR) between the uterine arteries (table 1). The analysis of qualitative indicators of uterine hemodynamics showed that patients of group 1 V max significantly increased in relation to the control group, against the background of a decrease in V min and an increase in the vascular wall IR. In group 1, an increase of V max by 2.1 times, IR – by 1.7 times, and the average value of V min decreased by 1.4 times in comparison with the standard data (P< 0.05), while significant differences with the parameters of group 2 have been obtained. Similar changes in hemodynamics in uterine arteries in uterine myoma in combination with hemorrhagic syndrome have been demonstrated in the work of I.E. Rogozhina et al. (2013) [15]. In the publication of D.V. Dzhakupov et al. (2014) presents the results of morphological studies of myometrium and myomatous nodes confirming the role of hypertension in the major arteries of the uterus in the pathogenesis of bleeding in myoma [5], which, in our opinion, is a consequence of increased IR of the vascular wall [9] and is consistent with the work of other scientists [6, 12].
In determining the local immune status in uterine aspirates in patients with complications of hormone therapy of uterine fibroids, an increase in the production of macrophage proinflammatory cytokines IL-1 (5 times) and TNF-α (4.5 times) in the endometrium has been found, against the background of the relative insufficiency of anti-inflammatory IL-4, the content of which increased only 2 times in relation to the control values (table 2).
In group 2, a slight increase in local IL-1 and IL-4 has been observed against the background of a significant increase in TNF-α (1.6 times in comparison with the control group). The resulting values of cytokines in the 2 groups had significant differences with the same parameters of the 1st group. According to some scientists, the increase in the production of local cytokines in the endometrium is associated with the inhibition of antitumor immunity, which leads to increased cell proliferation in the uterine myoma node and can contribute to the development of the cancer process [2, 7, 19].
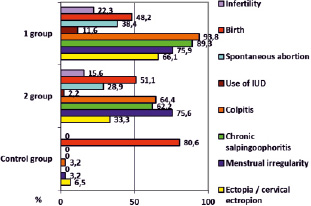
Fig. 1. Features of obstetric and gynecological history in groups
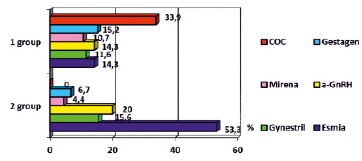
Fig. 2. Variants of hormonal therapy in groups
Table 1
Results of ultrasound and Doppler in the groups of women examined
|
Indicator under study |
1 group (n = 112) |
2 group (n = 45) |
Control group (n = 31) |
|
Average uterine volume, cm3 |
357,4 ± 14,51* |
349,8 ± 15,36* |
84,7 ± 5,22 |
|
Endometrium, mm |
8,3 ± 0,26*# |
2,6 ± 0,31 |
1,6 ± 0,03 |
|
Average maximum node size, mm |
27,16 ± 0,45 |
26,73 ± 0,34 |
0 |
|
Linear velocity of blood flow Vmax, cm / sec |
30,16 ± 1,10*# |
15,54 ± 0,09 |
14,16 ± 0,23 |
|
Linear velocity of blood flow V min, cm / sec |
5,41 ± 0,08*# |
7,59 ± 0,78 |
7,34 ± 0,14 |
|
Resistance index (IR ) |
0,82 ± 0,02*# |
0,48 ± 0,07 |
0,47 ± 0,02 |
Notes: * – differences of indicators in relation to the control group are reliable, P< 0.05;
# – differences of indicators in relation to group 2 are significant, P< 0.05.
Table 2
Results of the study of local cytokines
|
Parameters under study, pg / ml |
1 group (n = 112) |
2 group (n = 45) |
Control group (n = 31) |
|
IL-1β |
19,91 ± 0,33*# |
4,37 ± 0,07 |
3,83 ± 0,12 |
|
IL-4 |
3,06 ± 0,04*# |
1,72 ± 0,04 |
1,46 ± 0,02 |
|
TNF-α |
15,87 ± 0,28*# |
5,58 ± 0,13* |
3,51 ± 0,04 |
Notes: * – differences of indicators in relation to the control group are reliable, P< 0.05;
# – differences of indicators in relation to group 2 are significant, P< 0.05.
Hysteroscopy and visual assessment of the uterine cavity in patients with abnormal uterine bleeding clinic on the background of hormonal therapy of uterine fibroids in 25 cases has shown signs of endometrial hyperplasia. Endometrial atrophy has been found in 10 women in group 1, polyp – in 6. In other cases the visible signs of pathology of the endometrium with hysteroscopy have not been traced. The results of the morphological study of tissue samples after biopsy (fig. 3) have shown the predominance of the endometrium corresponding to the phase of proliferation in the event of hemorrhagic syndrome against the background of hormone therapy of uterine myoma (n = 46; 41.1 %).
The early stage of the secretion phase in the endometrium has been established in 21 patients. In each 5 cases, the endometrium corresponded to the middle stage of the secretion phase. Violation of the structure of tissue, characteristic of hyperplasia of the endometrium, demonstrated by 14 women 1 group. Glandular-fibrous endometrial polyp has been found in 6 cases. In addition, morphological criteria of chronic endometritis, manifested by the presence of follicular infiltrates, fibroplastic and ischemic processes in the basal layer and/or stroma of the endometrium, have been revealed in all endometrial samples in group 1. Plasma cells in endometrial tissue have been found in 102 samples (91.1 %). Incomplete morphological picture of chronic endometritis (with the absence of plasma cells) was only less than 10 % of the observations.
As you know, the dysfunction of the immune system plays a significant role in the emergence and progression of many diseases, including benign tumors. We have established a violation of the General immune status with the reduction of Th1 – and Th2-lymphocytes functions, as well as a significant inhibition of apoptosis in patients with uterine myoma complicated by hemorrhagic syndrome during hormone therapy [10]. In addition, in the publication of G. Wegienka (2012) suggested the hypothesis that uterine fibroids should be associated with disorders of systemic immunity against inflammatory diseases of the genital organs [17]. However, V.E. Radzinsky et al. (2016) suggested that chronic endometritis is characterized by an inadequate immune response to the presence of synanthropic bacteria that trigger autoimmune inflammation fueled by the persistence of legitimate microbes [14].
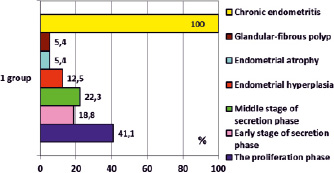
Fig. 3. The results of morphological studies of the endometrium in the 1st group
Conclusion
The results of the study have shown that the occurrence of complications of hormone therapy in uterine myoma is due to the presence in the history of inflammatory diseases of the internal genital organs (93.8 %). Hemorrhagic syndrome in uterine myoma is usually accompanied by an increase in the synthesis of proinflammatory cytokines IL-1b and TNF-α in the endometrium, against the background of the relative failure of anti-inflammatory IL-4 and hemodynamic changes in the uterine arteries, which can cause further tumor growth. Hysteroscopy with endometrial biopsy in combination with uterine fibroids with abnormal bleeding has revealed the presence of histological signs of chronic endometritis in 100 %, which confirms its role in the pathogenesis of complications of hormone therapy and is a pathomorphological explanation for the increase in the concentration of local cytokines in comparison with the control data. The obtained data dictate the need for a more detailed examination of women with uterine myoma before prescribing hormonal drugs to optimize existing standards and reduce the frequency of complications of hormone therapy.

