Infections of the genital tract are considered common causes of male fertility disorders, with a prevalence of 6-10 % [1]. Most of the affected men are asymptomatic [2, 3].
Urogenital chlamydial infection of lower genitourinary tract is of great interest today [4].
Today, chronic prostatitis is the most common urological disease in men younger than 50 years.
Special attention these days should be given to infectious prostatitis, which occurs on the background of chronic urethritis, often caused by C. trachomatis.
The diversity of the etiology and pathogenesis of this disease causes difficulties in the choice of therapy.
The purpose of this research is to study the effectiveness of treatment of patients with infectious prostatitis combining azithromycin, gemifloxacin and integrated therapy.
Materials and methods of research
The study included 104 patients with infectious prostatitis randomized in the main group (MG) – 53 men and the comparison group (CG) – 51 men.
In both groups the contingent workers from 33 to 50 years prevailed. Most patients were married. The duration of prostatitis often accounted for terms from 3 to 6 years (MG – 83.1 %, CG – 84.4 %).
The patients’ prostate glands were ultrasound tested, which confirmed the diagnoses and specified the nature of the changes in them. During the etiologic evaluation of patients the PCR (polymerase chain reaction) and the Real Time PCR were used. The cultural research was conducted to determine Tr. vaginalis and N. gonorrhoeae. The anaerobic flora in the content of the prostate gland was allocated. The level of testosterone, follicle-stimulating hormone and prolactin was determined by ELISA (enzyme-linked immunosorbent assay).
84.8 % of patients in the MG and 81.3 % in CG had serous secretions, often of abundant nature. 52.9 % in MG and 56.9 % in CG were diagnosed with anterior urethritis.
C. trachomatis were detected in almost half of patients in the form of monoinfection. In 20.8 % of patients in the MG and 21.6 % in CG had a combination of C. trachomatis and U. urealyticum. Peptostreptococcus and E. coli were most frequently found in opportunistic flora. In both groups’ patients with significant increase in the quantity of leucocytes in the secretions from the urethra prevailed.
When assessing symptoms of chronic prostatitis on NIH-CPSI (National Institutes of Health – Chronic Prostatitis Symptom Index), severe symptoms (30 to 43 points) were found with more than half of the patients in the MG (52.8 %) and CG (51.1 %).
Almost 60 % of patients in both groups had decreased volume of ejaculate. Normal motility of the cells was indicated in 8.3 % (MG) and 9.1 % (CG). Normal viscosity, respectively, in 33.3 % (MG) and 27.3 % (CG). Alkaline pH – 54.2 % (MG) and 45.4 % (CG). Only 47.2 % of men in MG and 49 % in CG had normal level of testosterone. The follicle-stimulating hormone, respectively, in 64.2 % (MG) and 62.7 % (CG); prolactin – 66.1 and 64.7 %.
In the study of deviations from normal levels of sex hormones in both groups (104 men), the correlation dependence levels of testosterone and follicle-stimulating hormone (r = + 0.66), testosterone and prolactin (r = + 0.56) were found.
The following regimen was developed: patients MG (n = 53) received 1.0 g of azithromycin per day on the 1st, 7th, 14th days, along with gemifloxacin 1 tablet (320 mg) per day for 14 days + complex therapy: suppository Vitaprost plus 1 per night for 10 days; prostate massage every other day 7 times; rectal laser therapy daily for 10 days. Treatment of patients in CG (n = 51) were distinguished by appointment of ofloxacin (1 tablet twice a day for 14 days) instead of gemifloxacin.
Mathematical processing of data was performed using Student’s t-test. Differences were considered relevant when t > 2, p < 0.05 – 0.01. The nature of the relations (r) between the studied indicators were established on the basis of correlation and regression analysis. Statistical processing of data was performed on a personal computer using the StatSoft Statistica v6.0 package.
Results of research and their discussion
One month after the treatment all patients had the eradication of C. trachomatis.
When comparing the dynamics of the parameters between the groups was found that the decrease in the number of conditionally pathogenic flora was statistically significant in MG.
According to the results of urethroscopy patients in MG had normalization of the mucosa of the urethra along its entire length 11.9 % more often than patients in CG (p < 0.05).
When examining the content of the prostate gland in men, the MG did not have a single patient with a significant increase in the number of leukocytes. However, there were 6 (11.8 percent) out of 51 of such patients in CG (p < 0.05).
The data ultrasound of the prostate gland was the objective indicator of the treatment effectiveness of chronic infectious prostatitis. One month after the treatment, the echostructure improvement of the prostate occurred in 44 out of 53 patients in MG and 33 out of 51 men in CG, which is 18.3 % less than in MG (p < 0.05).
The positive dynamics of the overall assessment of symptoms of chronic prostatitis (on NIH-CPSI) was also noted in both groups one month after the above treatment. Reliable positive changes in overall assessment of symptoms of chronic prostatitis (on NIH-CPSI) were more prominent in the MG compared to the CG.
Dynamics of previously impaired sexual function and the indicators of the level of sex hormones in blood serum and coagulation were positive in both groups. Although the number of patients with increased viscosity was reduced to 12.5 % in MG and 33.3 % in CG. The number of men with a normal volume of ejaculate was 75 % in MG and 68.2 % in CG.
Comparative analysis of the immediate results of the therapy developed by the scheme showed a more pronounced treatment effectiveness in MG compared to CG.
All patients were re-examined after 6 months of treatment (fig. 1).
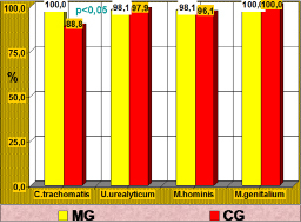
Fig. 1. The difference in the frequency of C. trachomatis detection between the groups after 6 months of treatment
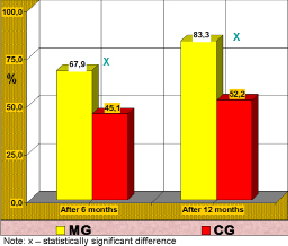
Fig. 2. The number of patients (in %) with low symptoms (on NIH-CPSI scale) of chronic prostatitis in 6 and 12 months after the treatment
C. trachomatis and M. genitalium were not detected in men of MG when examined on STI by PCR. M. hominis was detected in one patient and U. urealyticum in another. Among CG patients C. trachomatis was detected in 6 men (11.2 %), M. hominis in 1 (2.1 %). C. trachomatis was in association with U. urealyticum in one man of CG.
The difference in the frequency of C. trachomatis detection between the groups is statistically significant (p < 0.05).
In MG the number of patients with low symptoms of chronic prostatitis (0-14) on NIH-CPSI increased by 5 and reached 36 patients (67.9 %). In CG the number increased by 3 and amounted to 23 men (45.1 %).
In MG patients the normal number of leukocytes in the content of the prostate was found 22.2 % more often than in CG men (p < 0.05). There were 26.0 % more men in MG with normal echoes prostate (p < 0.01) and 22.8 % with low symptoms of chronic prostatitis compared to CG (p < 0.05).
Thus, in terms of up to 6 months 2 (3.8 %) of the 53 patients in the MG and 4 (7.8 %) of the 51 men in CG had the exacerbation of chronic prostatitis.
Statistically significant difference was found in the effectiveness of treatment after 1st and 6th month. It was 45.3 % higher in the MG (p < 0.01) and 35.2 % higher in CG (p < 0.01).
12 months after the treatment 48 men in MG and 46 in CG were examined. C. trachomatis and M. genitalium were not found when screening the MG patients for STI. M. hominis was detected in one (2.1 %) of the 48 people and U. urealyticum in another (2.1 %).
The CG patients were not detected with M. genitalium. M. hominis was found in 2 (4.3 %) of the 46 patients; U. urealyticum in one (2.2 %); C. trachomatis in one man (2.2 %). The analysis of the case of C. trachomatis detection showed that the infection was repeated.
12 months after the treatment patients (except the above mentioned) did not complain of anything. In this regard, the total score of chronic prostatitis symptoms (NIH-CPSI) was taken as the basis of therapy effectiveness. It turned out that the number of patients in MG with low symptoms of prostatitis increased by 4 and reached 40 (83.3 %) of 48 patients; in the CG the number increased by one and amounted to 24 (52.2 %) of the 46 men. The MG had 31.1 % more patients with a higher rate of therapy effectiveness (p < 0.01).
The comparative data of the treatment effectiveness of patients with chronic infectious prostatitis in both groups (on NIH-CPSI scale) in 6 and 12 months after the treatment is reflected in the fig. 2.
Thus, there was increase in the number of men with low symptoms of chronic prostatitis in the MG. Therefore, the combination of gemifloxacin with azithromycin in association with similar complex (pathogenic) therapy in both groups was justified.
Conclusion
The study demonstrated the effectiveness of the developed treatment regimens for patients with chronic infectious prostatitis in short-and long-term.
One month after the treatment patients in MG had the eradication of opportunistic flora in the content of the prostate gland secretion and normalization of the urethra mucosa more often than men in CG. Also the normal number of leukocytes from the mucous membrane of the urethra was 18.0 % more in MG (p < 0.05). There were more men with the improvement of the echostructure of the prostate and low symptoms of chronic prostatitis in men of MG compared to CG.
Positive dynamics of the above indicators had an impact on the level of sex hormones in blood serum, triglycerides, and the state of sexual function in favor of MG.
Long-term results of the treatment of patients were tracked. After 6 months of treatment C. trachomatis were not found in MG patients, while in CG 11.8 % had it. M. genitalium was absent in both groups. In a few cases U. urealyticum and M. hominis were detected in both groups.
Men in MG had the normal number of leukocytes in the content of the prostate 22.2 % more often than men in CG. The lecithin grains – 20.3 % more. Number of patients in MG with normal echoes prostate was 26 % greater and those with low symptoms of prostatitis 22.8 % greater (p < 0.05-0.01).
12 months after the treatment in MG C. trachomatis and M. genitalium was not detected. U. urealyticum was detected in one man (2.1 %) and M. hominis in another (2.1 %).
In CG M. genitalium was not found; M. hominis was detected in 2 (4.3 %), U. urealyticum in one (2.2 %); C. trachomatis in one patient (the later was re-infection).
Also in MG the number of patients with low symptoms increased to 83.3 %, while in the CG to 52.2 %, which is 31.1 % lower than that in MG.
These figures confirmed the validity of our combination of gemifloxacin and azithromycin for the effective treatment of patients with chronic infectious prostatitis.
This scheme can be used in practical health care.

