In well-developed countries, at the background of a continuous growth in injury rate, development of medical technology is mainly related to implementation of implants, produced of materials that have become called biocompatible (metals, ceramics, polymers). Most frequently traumatology uses metal bone and intraosteal implants. Within philosophy of AO/ASIF a wide range of various plates and pins for bone an intraosteal osteosynthesis of different bone areas has been developed as well as an original toolset. A great attention is devoted to solidity of the very fixator, as it receives all the strain before bone splinters are consolidated (several months).
During the recent years it has been recommended to treat diaphyseal fractures with implementation of intramedullary elastic pins with 2–4 mm of thickness, including those with bioactive covering [5, 8]. According to authors, it can stimulate reparative osteogenesis and reduce period of fracture union 2–4 times
The objective of this research is to explain the necessity of an implant osteointegration into bone-marrow channel for reduction in bone fracture consolidation period.
Materials and methods of research
Two series of experiments have been undertaken on mature breedless dogs of both sexes with body mass 20 ± 2,9 kgs. For the first series (n = 12) narcotized animals were exposed to intramedullary reinforcement of tibial bone with pin, made of titan alloy (Ti6Al 4V) 1,8mm thick, covered with hydroxyapatite (HA). After it fracture of bone diaphysis was modeled, and osteosynthesis with apparatus of Ilizarov was undertaken.
The animals were observed for 14–180 days after the surgery. Fracture union was defined according to roentgenologic indications and results of clinical sample. For clinical sample we removed the pins that were connected subsystems of Ilisarov apparatus, and splinters were then exposed to rotation and flexion strain. Lack of pathological mobility in the area of osteotomy was defined as criterion of union formation, and Illizarov apparatus was removed on that day. Pins that had been introduced into bone-marrow channel, were not removed during lifetime observations over animals.
Analysis of fracture union solidity was done according to biomechanical research at a special workbench, where the studied bone was strained with diametrical bending force from 1 to kgs. Degree of bone elastic bending was measured with micrometer of watch type – (IC25 class 1 GOST 577-68 GRIFF 017911, Russia) with evaluation accuracy ±0,01 mm.
For the second series (n = 5) we tested degree of osteointegration for intramedullary pins with bioactive cover, received via different technologies [10]. For that in each case one pin was placed intramedullary without fracture modeling and fixed for 4 weeks. After it the pin was removed with evaluation of tear off force with dynamometer DEPZ-1D-1U-1 (Russia) that has tension-resistance sensors that provide for evaluation accuracy ± 0,01N (animals were placed under narcosis, euthanasia was not implemented). Calculation of pin tear off force (P) was made according to the formula:

while F is tearoff force; L is pin length; d is pin diameter.
Statistic procession of quantitative data was made with implementation of paired binary t-test (p < 0,05) and criterion of Wilkinson for independent selections (p < 0,05).
The experiments were undertaken in accordance with “European convention on protection of vertebrate animals, used for experimental and other scientific purposes” (Strasbourg, 1986) and approved by Committee of ethics in Federal state budget institution “Russian scientific center “Recreational traumatology and orthopaedics” of academy member G.A. Ilizarov”.
Results of research and their discussion
During the experiment no oscillations in food and water consumption has been registered among the animals within clinical observation. Complications of neurological or infection nature did not happen. Supporting function of the tested segment preserved during the whole period of experiment. During the whole test intramedullary pins remains fixed, no shift in their position was registered.
Roentgenologic union of fracture came in 2–3 weeks of osteosynthesis. Our morphological research, published earlier, as well as computer tomography [7] confirms that a bone case is formed around intramedullary pin due to induced local osteogenesis (Fig. 1, b). Thickness of the mineralized wall in this “case” can reach 3 mm, and further it links firmly to endostome and bone-marrow channel is filled with spongy bone along the whole length of intramedullary pin (Fig. 1, a, c). This so-called bone “pin” provides for stability of bone splinters, quick consolidation of fracture, and possibility of complete strain upon the damaged limb for soon as one month after the surgery.
The results of tear of test for intramedullary located implants are presented in Table.
 a
a  b
b  c
c
Fig. 1. Preparations of tibial bone of a dog: а – in diametrials cut of wet preparation we can see that bone-marrow channel is filled completely with spongy substance of bone tissue; b – in diametrical cut of bone preparation after dissolution of organic component with spirit-ether composition (patent RF№ 2495567) we can see a clear “case” of local bone formation around intramedullary pin that is connected firmly to endosteel surface with trabecules; c – along the whole length of intramedullary pin we can see a formed bone “pin” – spongy substance of bone that has filled bone-marrow channel completely (trough spongy bone intramedullary pin is visible), the arrow points to a.nutricia (cortical layer is partially removed)
Level of effort during tearoff for pins with GA covering, layed via different technologies
|
Technology of pin GA covering |
Pin length (mm) |
Pin diameter (mm) |
Tearoff effort (H) |
Pin surface area (mm2) |
Tearoff effort (GPa) |
|
1. Steel + (polylactide, mixed with hydroxyapatite) |
44,25 ± 7,2 |
1 |
36,725 ± 2 |
138,72 ± 23,08 |
353,6 ± 11 |
|
2. Steel + Ti (titan layer + primer) + GA (microarc oxidation) + GA (high-frequency magnetron dispersion) |
60,66 ± 0,1 |
1,6 |
95,1 ± 4 |
304,79 ± 4,74 |
312,2 ± 20 |
|
3. Steel + Ti (titan layer-primer) + ГА (high-frequency magnetron dispersion) |
70,0 ± 17,8 |
1,4 |
126 ± 4 |
307,72 ± 78,22 |
421,0 ± 17 |
|
4. Steel + ГА GA (high-frequency magnetron dispersion) |
70,0 ± 13,5 |
1,8 |
203,5 ± 9 |
396,1 ± 76,0 |
400,6 ± 27 |
|
5. Titan + GA (microarc oxidation) |
81,75 ± 22,3 |
2 |
258,9 ± 9 |
513,3 ± 76,53 |
494,7 ± 28 |
|
6. Steel + (solopolimer of tetraphtoretilene with vinilidenphtorite, mixed with hydroxyapatite) |
71,4 ± 18,4 |
2 |
219,6 ± 7 |
419,2 ± 115,59 |
514 ± 20 |
|
7. Steel |
75,0 ± 8,2 |
1,6 |
14,09 ± 5 |
393,5 ± 41,02 |
351,1 ± 18 |
Test results show us that the least tearoff effort is typical for steel pins without covering (№ 7). The formed microporous calcium-phosphate layer at the surface of pins, produced of titan (technology-5) improves indexes of connection to the surrounding tissue by more than 140 % in comparison to pins without covering. Steel implants with composite signet-electric biologically-active covering (technology-6) with copolymer VDF-TeFE contents 35 % have shown stability of connection with bone tissue at a similar level as titan pins with covering, produced according to technology MDO.
Solidity of fracture union was defined with bench tests via exposing the damaged bone to bending strain. Clinical probe has shown lack of any bone fragment motion in the area of fracture. During the research at special bench (Fig. 2), when the bone was exposed to diametrical strain with effort from 1 to 8 kgs, degree of elastic bone bend did not exceed 0,6 mm.
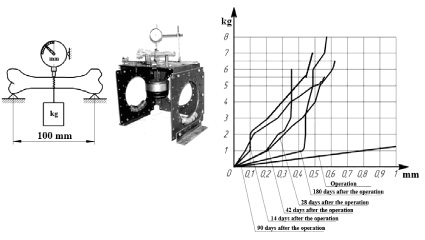
Fig. 2. Scheme of effort, test bench (picture), graph of dependence between bone shift and bending effort
We have undertaken evaluation test of maximum allowed effort upon a dog limb under intramedullary osteosynthesis of tibial bone with titan pin surfaced with bioactive covering after removing apparatus of Ilizarov. A number of allowances were made in calculation. Bone material was conditionally acknowledged as homogeneous, whole, and isotropic. It was considered that a “case”, formed around the pin from spongy bone substance, is connected with equal firmness to cortical bone layer and pin. Section of bone-marrow channel was acknowledged as round. Solidity limit for tension and contraction of spongy bone tissue was taken as σ = 6,2 MPa, and elasticity module was taken as E = 200 MPa [1], module of pin material elasticity – 400 MPa [2]. The allowed tangent tension of spongy bone tissue was taken as 3,4 MPa according to condition
[t] = 0,55•[σ].
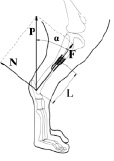
Fig. 3 presents scheme of strain upon dog limb during tread that was used in calculation.
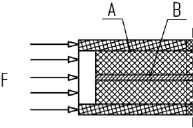
Under the impact of strain P in the area of fracture several types of tension emerge, such as tension of contraction, bending, and shift. Scheme of fracture area strain under contraction is presented in Fig. 4, a.
Contraction of fracture area takes place in longitudinal component F from effort P that was defined according to condition F = P•cos?. In spongy bone substance tangent and normal tension emerges, it causes cut and contraction.
Tangent strain was defined through equation:
t = F/S,
while F is longitudinal component of force P;
S = c•π•d2 = 1,4 sm2
is the area of cut surface. A dangerous surface for cutting was considered area of contact between bone post and pin (area B, Fig. 4, a), as there area of contact is smaller than area of contact between bone post with cortical layer (area A, Fig. 4, a). Utmost allowed strain upon the cut in the area of pin contact:
F = [t]•S = 48 kgs.
For the area of contact between bone “pin” with compact bone substance area of cut surface was defined as S = 18,8 sm2, utmost allowed strain upon cut equals F = 640 kgs.
Normal strains were defined from equation
σ = F/S1,
while S1 is the area of bone “pin” cut.
S1 = π•r2 – S2,
while r is radius of bone “pin” 10 mm, and
S2 = π•r2
is area of pin cut (r is pinъ radius 0,75 mm). Utmost allowed strain of contraction:
F = [σ]•S1 = 193 kgs.
Criterion of fracture place solidity for general strain upon limb P is defined as utmost allowed strain of contraction for bone post. When this strain is achieved, collapse of bone post and its cut off will take place under the impact of longitudinal force component. Utmost effort upon the limb equals P = 205 kgs.
 a
a 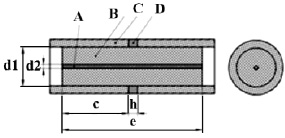 b
b
Fig. 3. Schemes: a – strain upon animal limb during tread, while P is supporting strain upon limb; N is diametrical component of force P; F is longitudinal component of force P; L is arm of N force impact, acknowledged as 10 sm for calculations; α is angle of limb oscillation during vertical tread, acknowledged as 20° for calculations; b – scheme of bone fracture area: A is pin, B is spongy bone (bone post), C is cortical layer, D is bone regenerate, d1 isdiameter of bone post; acknowledged as 2 sm for calculations, d2 is pin diameter, acknowledged as 0,15 sm for calculations, e is length of bone post, acknowledged as 6 sm for calculations, c is length of contact area between bone post with cortical layer of bone fragment, above and beneath fracture, acknowledged as 3 sm for calculations, h is fracture area
 a
a 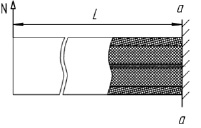 b
b
Fig. 4. Scheme of fracture area strain with longitudinal effort (a); bending diametrical force (b)
Bending of fracture area (Fig. 4, b) takes place under the impact of diametrical component N of effort P that creates bending momentum
M = N•L,
while N = P•sinα.
In diametrical cut impact of bending momentum M creates tension of stretching and contraction. Normal tensions in case of bone post (“pin”, “case”) bending are
σ1 = M•r/J1 [9],
normal tensions in case of pin bending are
σ2 = M•r/J2,
while r is bone “pin” radius, or pin radius is used in corresponding equations, J1J2 are inertia momentums of cut area for bone post and pin correspondingly.
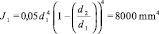
for bone post,

for pin. Utmost allowed bending effort for bone substance is
N1 = σ1•J1/L•r = 4,9 kgs;
for pin bending
N2 = σ2•J2/L•r = 0,13 kgs.
As the dangerous cut contains materials with different characteristics, equation of calculating two-layer beam bending was implemented: for bone “case”
σ1 = M•r•E1/(E1•J1 + E2•J2);
for pin
σ2 = M•r•E2/(E1•J1 + E2•J2).
Effort that creates critical internal tension under bending was calculated:
for bone substance:
N1 = [σ1]•(E1•J1 + E2•J2)/L•r•E1 = 5,4 kgs;
for pin:
N2 = [σ2]•(E1•J1 + E2•J2)/L•r•E2 = 7,7 kgs.
Therefore, under the impact of effort P critical values of internal tension will take place in spongy bone from diametrical component of N that bends the bone. Criterion of fracture area solidity was considered as the minimal of utmost allowed forces that create effort P, in other words, bending force N 5,4 kgs that impacts bone post and can emerge under the allowed force P = 15,7 kgs.
The basic principle of modern bone and intraosteal osteosynthesis is mechanical positioning of damaged bone fragments in fixed condition until complete recovery.
Combined osteosynthesis of fractures in long tubular bones with apparatus of Ilizarov and intramedullary pins with GA covering has demonstrated us the possibility of bone union in clinical conditions in 3–4 weeks. It is known that hydroxyapatite covering induce bone formation around an implant and thus provides for larger area of contact between the pin and damaged bone, improving its fixation practically without any gaps between bone and implant [9].
The basic objective of research, related to implementing implants in orthopaedics and surgical stomatology is achieving the corresponding implant fixation in the surrounding bone. Evaluation of fixation degree is preferably performed with mechanical tests that allow researchers to receive quantitative indications [3]. Nowadays evaluation of mechanical characteristics of extracted implants is made via different methods. Tests for ejection and tearoff are simple and can be performed with cheap equipment [6]. After T. Nakamura developed an original method of tearing off an implant with bioactive surface from bone bed in 1985, several researchers of Kioto university have undertaken this test to evaluate firmness of connection between bone and various biomaterials, such as bioactive ceramic, titan alloy, covered with bioactive materials, chemically and thermally processed titan [4]. Their experiments demonstrated that connection between bone and implant increased with time for all materials except for clear titan. The highest level of implant tearoff was observed during implementation of glass-ceramic and, as well as in our research, dense hydroaxyapatite – around 80 newton, but only in 24 weeks of fixation and for contact area around 150 mm2.
According to technology of osteosynthesis and biomechanical conditions that are created in the area of fracture, all implants can be divided into static and dynamic. For static (shunt) osteosynthesis the most of strain lays upon fixator. It leads to a number of negative effects: osteoporosis in not-strained area of bone, decrease in efficiency of osteosurgery in the area of fracture, and also increase in risk of implant and bolt collapse. Dynamic osteosynthesis that is usually implemented in the second half of treatment process (after several months, when slow consolidation is diagnosed), allows specialists to distribute strain between fixator and bone thus stimulating reparative ostheosynthesis in fracture area. Degree of strain distribution depends on a number of conditions and is not regulated in process of practical implementation.
From our point of view exclusion of all unfavourable conditions for union during osteosynthesis can take place in case of maximal osteointegration of implant, and it requires increase in their biological activity. Even such insignificant in it diameter intramedullary implant as a pin with GA covering establishes optimal conditions for fracture consolidation in 2–3 weeks [7]. At the same time, solidity of connection between the pin and bone endostome can endure tearoff tension over 500 GPa.
Mathematical calculations show us that criterion of fracture area stability against impact of force P upon a limb is utmost allowed bending effort. In our case safe effort upon the limb after 2 weeks of osteosynthesis, provided by bone post and pin, equaled 15,7 kgs. The formed bone case (post) covered the area of bone fracture and provided for increase in solidity of bone in this area, established limb supportability at the final stage of fracture union.
For an experimental animal, in our case – a dog weighed around 20 kgs, which weight is distributed between 4 limbs during calm tread (5 kgs per limb), effort is 2 times lower than allowed, and for clam walk on 2 limbs (10 kgs each) it is also lower than allowed. In this regard we observed no limb deformations after removal of Ilizarov apparatus even so soon as 2 weeks after the surgery.
If we undertake biomechanical calculations for human bone, we can see that with implementation of a combined osteosynthesis with intramedullary bioactive implant a traumatologist can expect solidity of shin consolidation for a patient even in case of early removal of Ilizarov apparatus against longitudinal strain above 180 kgs, and stability against cut above 100 kgs. Bending effort with force close to 39 kgs can result in secondary fracture, therefore, additional preventive immobilization of the damaged segment is possible in shape of orthesis that will reinforce the limb and increase the allowed strain upon it, resisting bending.
Conclusion
An optimal method of intraosteal osteosynthesis for fractures of long tubular bones is osteosynthesis at the foundation of implant osteointegration. A guaranteed process of osteointegration establishes bioactive layer at the surface of implant in shape of hydroaxyapatite. Such approach towards fracture treatment allows for a significant decrease in width and mass of an implant, thus preserving marrow and bone endosteum during surgery. Injury rate during surgery is decreased significantly and, at the same time, time period, required for fracture consolidation, decreases down to 2–4 weeks. Solidity of bone union allows for longitudinal strain upon limb more than 180 kg.
Research material is prepared with financial support of Russian scientific fund (project № 16-15-00176).

